As told by Nannette: 
I have to tell some back story first. I never wrote my birth stories for my first two children, which I plan to rectify starting here.
Jonah was my firstborn. I had just finished my nurse-midwife training program and taken my board exams. That was a long grueling 3 years, during which I got pregnant and miscarried. I discovered I was pregnant with Jonah just weeks after I passed my midwifery boards. The news arrived the same day our miscarried baby would have been due. Bittersweet. I was a young midwife just starting her homebirth practice, and I knew immediately I would have a homebirth with my son. My mother had cesareans for all 3 of us. But it was for a known problem related to an auto accident messing up her pelvis. I never doubted that these strong Irish hips could handle childbirth. There were not many choices of midwives in my area, but we settled on a very nice midwife and started the journey. I convinced my husband, who had just started his first full time job, to invest the time in Bradley classes (along with my best friend who was going to be at my birth as support and photographer). Things bumped along, I was having a healthy pregnancy and was busy with side jobs while I started my little homebirth practice. My due date came and went, but no biggie, I was a primip. Weekly visits with the midwife became concerning, though, as my son did not engage in my pelvis as he should have. When I passed the 42 week mark, and he was still not engaged despite regular bouts of prodromal labor, I went to see my “backup” hospital midwife on a Wednesday afternoon at 4pm. We had a BPP done, and it wasn’t great. And they told me Jonah (I found out he was a boy at this point) was 12.5 lbs, which frankly scared me as a first timer. And he was still not engaged. And my hospital midwife, who had been my preceptor in midwifery training, looked at me and bluntly said, ” you know the answer, Nannette. You just need to make up your mind.” I cried and asked to be induced (which wasn’t a good idea because he was so high in my pelvis and showing signs of stress), and then I accepted that my son was going to be born by cesarean. I looked at the doctor and asked to have it done right away. “If I go home, I don’t know if I can make myself come back.” So Jonah Graham was born at 7:21pm on June 29th by cesarean section weighing 10lbs8oz. It was a surreal experience. I was on automatic pilot for a lot of it. One thing I remember the most was how I panicked and almost cancelled the plan when I was getting the spinal anesthesia (they stuck me several times and kept hitting a nerve, which was excruciating and nearly sent me into a panic attack). The spinal finally took, I got draped and swabbed, the docs did their thing, and when I heard them lift him out of my stomach I didn’t breath again until he cried. And then I let myself break down. That was the start of a long, dark slide into postpartum depression. A story for another day.
Fast forward 10 months. I am in the middle of getting help for the PPD when I become pregnant again. We had treated Jonah for torticullis and we linked his malposition to an injury that I had had around 36 weeks that apparently had really torqued my pelvis. So with regular chiropractic care I was confident this was a problem that would not repeat itself. I was working with a midwife that was confident in VBAC (vaginal birth after cesarean), and I decided to plan a homebirth for my second baby. I worked through the PPD and the emotional issues that surround having a VBAC, and reached 36 weeks with our baby girl. She turned breech at that point, and it forced me to stop working and pay attention to her. We did 2 weeks of alternative/complementary techniques and successfully turned her back to head down. I then got extremely ill from the flu about a week before her due date. Not cool. In hindsight, I should have been hospitalized. On Easter Sunday, my 40 week mark, we were eating dinner with my husband’s mother, and contractions began. They felt like the prodromal ones I’d had with Jonah, which was encouraging! They slowly intensified through the night, and at 7am the next morning I was dealing with them in the living room and prayed for a clear sign because I wasn’t sure if I was being a wuss about them or if I was really in labor. Than, hallelujah, my water broke! It was on! My labor had started spontaneously at 40 weeks and 1 day! Major VBAC milestone! I was in active labor by late morning, but it was a really rough day. I constantly vomited and became dehydrated, and also had some terrible pelvic pain which even the chiropractor could not resolve with a visit while I was in labor. I reached 8 cm and the contractions started to wane. I nearly fell asleep in the pool. And it wasn’t the good sleep that midwives are thankful for, a pause to gather yourself. It was an exhaustion borne of utter depletion. I called my birth team and said, “I know I can do this. But I don’t think I can do it here.” And with that we called the hospital, praised God that Dr. Baltierra was on, and I counted in my head the 4 contractions I would endure in the car for the ride to the hospital. I got to JMH, checked in, got an epidural, eventually got an IUPC and pitocin to get contractions going again, and about 5 hours after I arrived at the hospital I woke up in a panic because the epidural WASN’T WORKING ANYMORE!!! And lo and behold I was complete and ready to push! They hiked me up and got out the mirror and at 5:39am on April 2nd, 2013, I pushed my beautiful 10 lb daughter out in 20 minutes! I did it! I birthed vaginally! And then I blacked out when I sat up to nurse and we discovered I had been severely anemic, probably an effect of the severe flu I should have been hospitalized for, and I had to get blood transfusions even though I had hardly bled with the birth. I also suffered some SPD damage and couldn’t walk normally for several weeks. But it was worth it for my VBAC!!
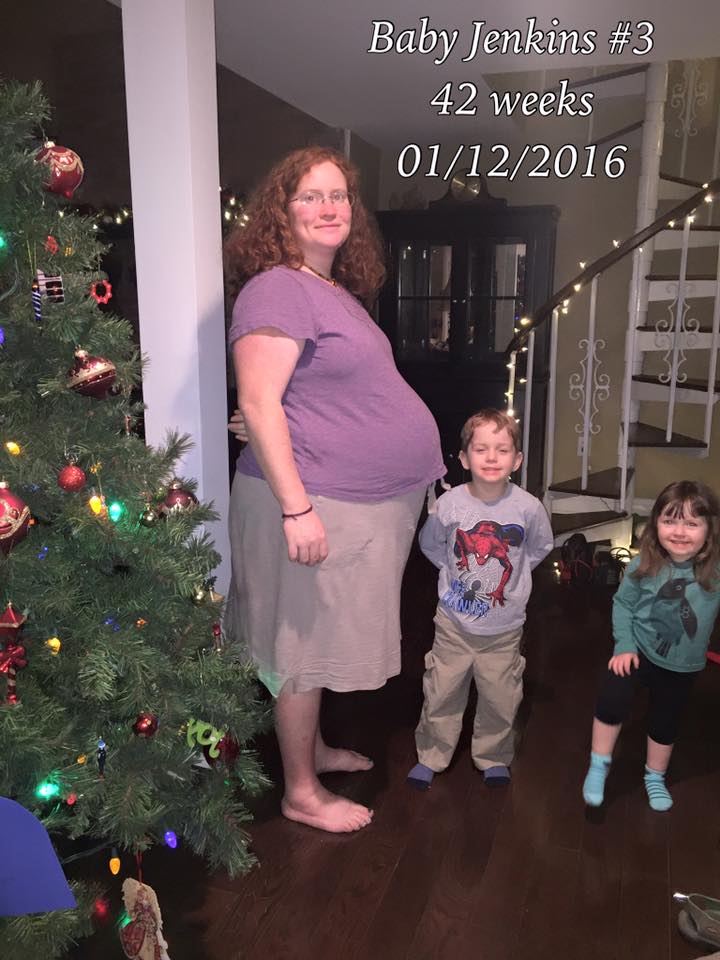
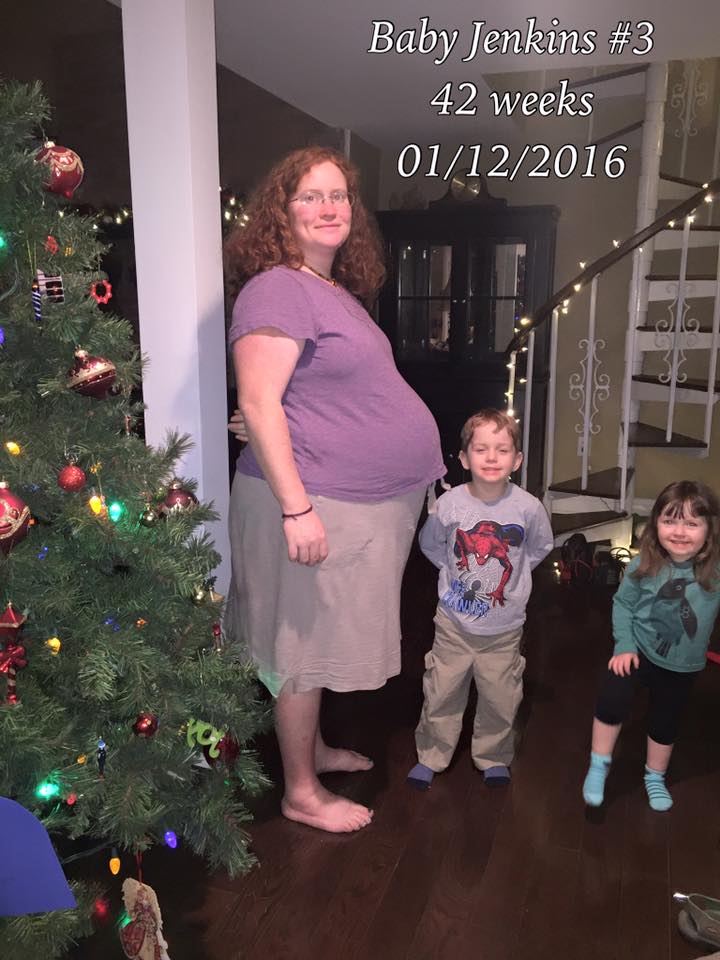
So fast forward 2 years. I was a very busy homebirth midwife at the time. I had recently gone through some very stressful transitions in my business partnership, and was praying for a year without change, just some stability so I could heal from the pretty bad emotional trauma. My daughter was weaning, and I knew that a pregnancy was possible soon. I am lucky enough to not ovulate until my babies stop nursing altogether. My cycle started, and repeated, and as the third round was finishing I looked at my husband and said, “all bets are off, you know.” We didn’t attempt to prevent, and sure enough, there was a positive. As stressful as it was, I was also thankful for the gift of another baby. I knew I would not be able to keep up the pace I was at with another child, and made the decision at that point, after a lot of prayer and counsel, to grow my homebirth practice instead of close it. God was watching out, and at the same time I decided I would hire one or two midwives, I was contacted by 2 midwives who were just what I wanted for Riverside. So I entered the second trimester with a good plan for work/family balance and the knowledge that this time I was going to get a proper maternity leave. I was so thankful for a healthy pregnancy. It was the best of all of them. I had good help, I was getting good sleep and exercise, I didn’t gain weight until the last few weeks. My belly measurements were consistently on track, which was better than my first two pregnancies which had always measured ahead, so my midwives thought this baby was going to be smaller which was nice to think of having had 10+lb’rs. I had amazing community support and was shown so much love by truly incredible women I am blessed to know and work with! I even got a surprise mother blessing! Jonah and Tabi were in love with the baby and so interested and involved in the pregnancy. I had an ultrasound but the baby wouldn’t play the gender reveal game, so it was really a surprise! We had a boy name and a girl name, Jonah and Tabi were excited to be there for the birth, and my midwife was really wonderful for me, a great pregnancy all around. I was “due” December 29th, so Jonah was expecting a Christmas time baby which just blew his 4 year old mind with anticipation. Christmas came, and went. New Year’s came as well, and went. The week after came. And went. And the mind games that accompany going overdue began. Thankfully, this was not my first VBAC, I knew my body was quite capable. And I thought this was a boy baby, so I figured maybe my boy babies just go late. I was encouraged and supported, and got wonderful help from friends and my fellow birthworkers during this time. I didn’t do anything really aggressive to start labor as I wasn’t worried over anything. I was fine, baby was fine, it was just taking a bit. I had a cervical exam at 41 weeks or so, and it was favorable, and I got a BPP done at 42 weeks, and it was just fine. But going overdue is emotionally taxing, and I cried on more than one morning when I woke up still pregnant. I worked on a labor music list. I crowd sourced some suggestions for music with a heavy bass line that would just carry you along without thinking. I didn’t to think too much. I’m a midwife, and know a lot, and I didn’t need to go down certain lines of thought. I was fine, baby was fine, my midwives were relaxed, I was just gestating a while.
On a Wednesday evening April 13th, 42 weeks and 1 day, I had some regular almost-contractions, and we inflated the pool just in case. But Thursday morning, I woke up well slept and still pregnant. On Friday evening, some good friends took my kids to the local Backyard Inflatables while I got acupuncture. I was relaxed, and we made plans to get some Glory Doughnuts for breakfast the next morning. You should definitely get doughnuts from them some time. Ah-mazing. So Saturday morning, January 16th, I woke up around 6am. The house was quiet, and I felt like getting up and just hanging out by myself. I had a few of the usual braxton hicks as I was sitting in my rocker petting one of the cats. I noticed they had some good pelvic floor pressure to them, which was an encouraging thought as that meant baby’s head was where it should be. But they were just BH as usual. My husband got up around 8:00, kids were sleeping in from getting worn out playing the evening before. We did a few chores, and I mentioned the doughnuts plan. So he left at 9:00 to get some. I took a picture of my sweet sleeping kids, climbing up on the bunk bed (timestamp 9:26am). No contractions. Just a nice, quiet Saturday morning. My midwives texted to check in. One midwife mentioned coming by to do some things to maybe encourage labor. I let her know I’d had some braxton hicks that had a little pressure to them, but that my kids weren’t awake yet so I didn’t think labor would start knowing they were about to get up. Then, I had one. A painful contraction. Not too long, but definitely different. Jonah woke up at 9:40, came downstairs. I had another one. I sent him to watch some cartoons and realized I had been a little short tempered with him. I had another one. I decided to go upstairs, and couldn’t get up the stairs before another hit. Well, well! I made it to my bathroom and texted my husband, “on your way back?” (timestamp 9:57am). My midwife texted a two part question, and I barely had time to text back “yeah”. (she later said she immediately knew it was time to come, that was not a usual texting style for me). Within 20 minutes of the first contraction I was in full blown labor. I could only stand, I had the sudden fear of my water breaking in my pants and undressed. I started vocalizing. I remember thinking vaguely “if it feels better to make noise then I must be in active labor?” The contractions hurt. A lot. And were fast. I couldn’t time them. I couldn’t text or call anyone. I couldn’t do anything. I tried to kneel, and couldn’t handle being bent and stood right back up. I paced around the bathroom, and kept saying in an attempt to keep myself grounded “this is how babies are born, this is how babies are born, oh God, this is how babies are born” as I experienced huge amounts of pressure with seemingly eternal contractions with hardly time to breath twice between them (later the chart said they were 90 seconds long and 30 seconds apart, so I wasn’t imagining it). My husband got up there, got the pool filling, got the babysitter and photographer on the way, texted the midwives (or called) to make sure they were enroute. In short he did a great job getting things in place and rolling. I starting feeling lightheaded and a little panicky, the contractions were even stronger. Chris, one of my midwives, arrived at 10:40. I started to cry and kept saying they hurt. She was very calm, listened to baby with the doppler, and started getting things out. She encouraged me to try to get in the pool. I felt locked in standing mode, afraid to move lest the contractions get EVEN stronger. But I managed to scoot over to the pool and climb in (at 11:00 per the chart). As I sunk into the water the next contraction crested. That was kind of awful. The feeling of my belly getting buoyant but then getting driven down in the contraction. The next one was better though, and I settled into the pool. The contractions got a little more spaced, maybe a minute apart, but then I started feeling them in my legs. Thankfully I was in the water, the pain in my thighs wouldn’t have been great with standing up. I complained. A lot. And cried, and repeated that things hurt and that I couldn’t do this forever. But I mostly had my eyes closed and my face down making lots of noise. A little after 11:00 I looked up and Lindsey, my photographer, had arrived. Grace arrived at that point, too. Grace has been with me a long time. My first birth assistant when I started catching babies while pregnant with Jonah. My doula for Tabi’s birth. My friend. And planning to catch this baby as my student midwife.

Bradley was there (I made a point to clock his presence as I had actually blanked out his presence at Tabi’s birth).

I looked up at some point and saw Jonah sitting on the side of the bed watching me labor. Mary was there, my good friend and my children’s nanny, I never worried about Jonah and Tabi being cared for.
At this point I feel like I was being dramatic but just needed to be allowed to not have my s*%^ together for once. This labor felt like a tsunami and I was just rolling around in the water underneath. I think I repeated that I couldn’t do this for 6 more hours and Grace assured me it wasn’t going to be that long. After what seemed like FOREVER my water broke (timestamp 11:10). My midwife voice automatically asked if the water was clear, which it was.

I had some urge to push with that contraction. And then I had a blessed, blessed, 2 minute pause. I came up for air. My head cleared. I thought, and I think I said, “I can do this part. I know how to push.” Because I did. I revisited how I had pushed Tabi out in 20 minutes, my first vaginal birth. And how proud I had been (and am) of that. I had no idea how long I had been in labor for, but now it was time to push and I came back to center. Everyone was quiet. My ears were kind of ringing. I don’t know how loud I was on the outside, but there had been a whole lot going on in my head and it had all stopped. That long, blessed, 2 minute break. And then the contraction came and the deep, throat/abdomen/pelvic “HUHHHH” started. My body was pushing. A couple of contractions, and I clearly felt the round head of my baby descend. It did not feel like pooping. It felt like a large round hard thing moving down in my pelvis. That was my baby’s head! I hadn’t felt this with Tabi, being on the epidural. It was AMAZING to be aware of it. I felt some burning and said something like “am I crowning?! Please tell me I’m crowning!”, to which there was no reply. Crickets. “Crap, I’m not crowning…” Next contraction. There was some burning, which I clearly identified to be at the place I had had a minor tear with Tabi’s birth. I was ok with that. I was breathing through these. Not really on purpose. I was just trying to ride these suddenly close again contractions that were pushing my baby out. All of my energy was focused, I had to stay stretched out, one hand out on the side of the pool, body extended back. A straight path for the baby. Nothing in the way. My body doing its thing like I’d know from my first pregnancy that it could. I breathed and grunted and didn’t add any pushing effort and the baby came down and around and I felt the head birth. So amazing. I heard Jonah and Tabi’s voices, they were there at the pool side and saw the baby’s head and face. I had really hoped they would have that experience of seeing their sibling enter the world.

A minute passed, and another. I felt midwives’ hands back there. No one was worried, though I wasn’t really looking at faces, and I wasn’t worried. I did have the sudden thought that this had been long enough and it was time to push baby out. So I did push to finish the birth. And then I heard those words, “grab your baby!” I reached down, and glimpsed cord around the baby’s neck as Grace did, we turned baby in the water to unwind the cord and bring baby up.
And there she was. My baby girl. Born at 11:27am, less than 2 hours from the first recognizable contraction. “It’s done!” She took a minute to breath. It had, after all, been a fast birth. I gave her some puffs and stimulation to her back and feet she drew in her first air. Grace helped her with some postural drainage. I cried and thanked God it was over.

Tabi was absolutely thrilled that it was a girl!! “It’s a girl, it’s Saoirse!”

And she lifted her sweet little hand up and my baby was with me. Oh lordy. The tears <3
She weighed 9lbs 4 oz, nearly a pound less than my others. My postpartum experience was worlds away better. Resting in my own bed, being well taken care of, my children coming to see their baby sister. Normal, unhurried, quiet. As a midwife, I work hard to provide this experience to families. And I had finally had it myself. It was truly my best birth. And one of the best times of my life.

Something came up the week after the birth that I want to include here. There is a blog that I follow, Birth Without Fear, by a woman name Jan. Last year she had described being pregnant again; she had had cesareans, than a VBAC, than another baby, and was planning a homebirth again. She went overdue, and one morning woke up and knew it was time to have her baby and had a walk in cesarean. She felt empowered, she owned her decision and experience. But she described having an emotional breakdown just before the surgery, and how she had realized based on her past birth experiences that she was transitioning emotionally at that moment as she was getting ready to meet her baby. It was an incredibly healing read for me. I had experienced labor in all its raw, unmediated strength. I had “lost it” for a bit, felt panicky, cried, let out a lot of emotion. And I realized that I had done that before with Tabi’s birth, when I woke up panicky and ready to push. And I realized that the moment when I almost broke down while preparing for Jonah’s surgical birth HAD BEEN MY TRANSITION MOMENT. Realizing that connected all my births. It healed something I thought I had been over in my experience with Jonah. I did birth him. I went through the depths emotionally, though not necessarily physically. I realized I had carried some shame about how I almost had a panic attack with the spinal being inserted at Jonah’s birth. And with waking up all freaking out at Tabi’s birth. But those were my transition moments. It’s just what I do. I have to let go for a minute. And just let things happen. And just birth my babies.

Birth photos credit: Lindsey Welch Photography
———–
Click HERE to learn more about the Community Birth Stories Project or to submit your own birth story.